Hesi case study aortic regurgitation – The HESI Case Study on aortic regurgitation delves into the complexities of this cardiac condition, providing a comprehensive analysis of its pathophysiology, diagnosis, management, and outcomes. This in-depth exploration aims to enhance the understanding of healthcare professionals and students, empowering them to make informed decisions in clinical practice.
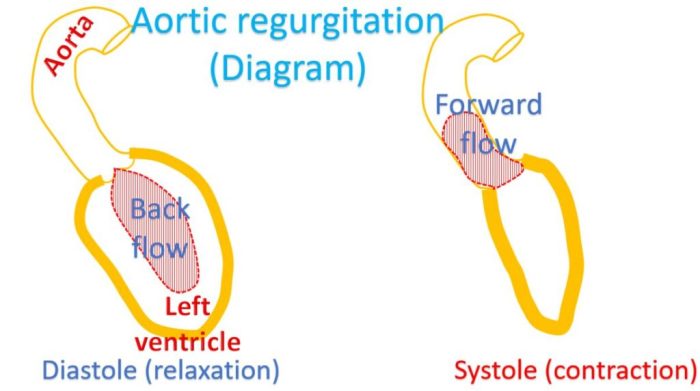
Aortic regurgitation, characterized by the backward flow of blood into the left ventricle during diastole, poses significant challenges in patient management. This case study provides a thorough examination of the underlying mechanisms, hemodynamic consequences, and clinical presentation of aortic regurgitation, laying the foundation for effective diagnosis and treatment strategies.
Pathophysiology of Aortic Regurgitation: Hesi Case Study Aortic Regurgitation
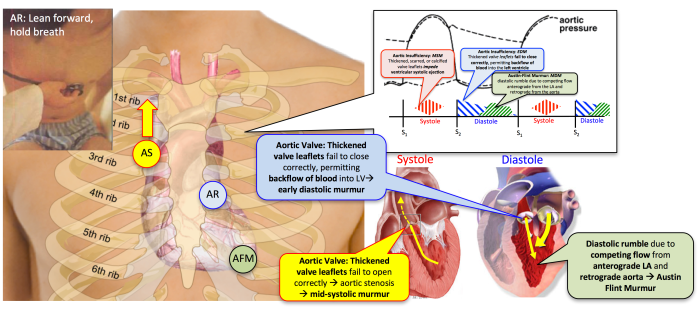
Aortic regurgitation (AR) is a condition in which the aortic valve fails to close properly during diastole, resulting in the backflow of blood from the aorta into the left ventricle.
The most common cause of AR is rheumatic fever, which leads to scarring and thickening of the aortic valve leaflets. Other causes include congenital heart defects, infective endocarditis, and degenerative changes associated with aging.
Mechanisms Leading to Aortic Regurgitation
The mechanisms leading to AR can be classified into two main categories:
- Structural abnormalities of the aortic valve:These abnormalities can include leaflet prolapse, perforation, or tears. They can also result from valve stenosis, which leads to increased pressure on the valve leaflets and can cause them to become deformed.
- Functional abnormalities of the aortic valve:These abnormalities can include impaired leaflet coaptation, which occurs when the leaflets do not meet properly during diastole. This can be caused by a variety of factors, including left ventricular dilatation, which can stretch the aortic valve annulus and prevent the leaflets from closing completely.
Hemodynamic Consequences of Aortic Regurgitation, Hesi case study aortic regurgitation
The hemodynamic consequences of AR depend on the severity of the regurgitation. In mild AR, the regurgitant volume is small and the left ventricle is able to compensate by increasing its stroke volume. However, in severe AR, the regurgitant volume is large and the left ventricle is unable to compensate.
This can lead to left ventricular dilatation, hypertrophy, and eventually heart failure.
Clinical Presentation of Aortic Regurgitation
The clinical presentation of AR can vary depending on the severity of the regurgitation. In mild AR, there may be no symptoms. However, in severe AR, symptoms can include:
- Dyspnea
- Fatigue
- Chest pain
- Palpitations
- Syncope
On physical examination, patients with AR may have a wide pulse pressure, a bounding pulse, and a diastolic murmur.
Diagnosis of Aortic Regurgitation
Accurate diagnosis of aortic regurgitation is crucial for timely and appropriate management. The diagnosis is based on a combination of physical examination findings, echocardiographic evaluation, and other imaging modalities.
Physical Examination
Physical examination plays a vital role in the initial assessment of patients suspected of having aortic regurgitation. The following findings are suggestive of the condition:
- Palpation:A palpable thrill over the aortic area, known as Corrigan’s pulse, is a classic sign of severe aortic regurgitation.
- Auscultation:A high-pitched, blowing diastolic murmur along the left sternal border, known as Austin Flint murmur, is characteristic of aortic regurgitation.
- Peripheral Signs:Wide pulse pressure, capillary pulsations (Quincke’s sign), and head bobbing (Musset’s sign) may be present in severe cases.
Echocardiography
Echocardiography is the cornerstone of diagnosing aortic regurgitation. It provides detailed images of the heart structures, allowing for the assessment of:
- Valve Anatomy:Echocardiography can visualize the aortic valve leaflets, assess their mobility, and detect any structural abnormalities.
- Regurgitant Jet:Color Doppler echocardiography demonstrates the regurgitant jet and provides information about its severity and location.
- Left Ventricular Function:Echocardiography evaluates left ventricular size, function, and the presence of any compensatory mechanisms.
Other Imaging Modalities
In certain cases, other imaging modalities may be useful in diagnosing aortic regurgitation:
- Transesophageal Echocardiography (TEE):TEE provides a clearer view of the aortic valve and can be helpful in cases where transthoracic echocardiography is inconclusive.
- Cardiac Magnetic Resonance Imaging (CMR):CMR can provide detailed anatomical information about the aortic valve and quantify regurgitant volume.
- Computed Tomography (CT):CT angiography can assess the aortic root anatomy and detect any associated abnormalities, such as an aortic aneurysm.
Management of Aortic Regurgitation
Aortic regurgitation management involves both medical and surgical approaches. The specific treatment plan depends on the severity of the regurgitation, the patient’s symptoms, and their overall health status.
Medical Management
Medical management is typically recommended for patients with mild to moderate aortic regurgitation who are asymptomatic or have minimal symptoms. It aims to slow the progression of the regurgitation and prevent complications. Medical management options include:
- Antibiotics:To prevent endocarditis in patients with severe aortic regurgitation.
- Vasodilators:To reduce afterload and improve cardiac function.
- Diuretics:To manage fluid retention and reduce symptoms of heart failure.
Surgical Options
Surgical intervention is indicated for patients with severe aortic regurgitation who are symptomatic or at high risk of complications. The primary surgical option is aortic valve replacement, which involves replacing the damaged valve with a prosthetic valve.
Perioperative Management
Patients undergoing aortic valve surgery require careful perioperative management to minimize risks and optimize outcomes. Key aspects of perioperative management include:
- Preoperative evaluation:To assess the patient’s overall health status, optimize medical conditions, and plan for surgery.
- Intraoperative monitoring:To closely monitor the patient’s vital signs, hemodynamics, and cardiac function during surgery.
- Postoperative care:To provide supportive care, manage complications, and monitor for signs of infection or bleeding.
Outcomes of Aortic Regurgitation
Aortic regurgitation, if left untreated, can lead to a spectrum of outcomes ranging from asymptomatic to severe heart failure and death. The natural history of the condition is highly variable, and the prognosis depends on several factors, including the severity of regurgitation, the underlying cause, and the patient’s overall health status.
Factors Influencing the Prognosis of Aortic Regurgitation
The prognosis of aortic regurgitation is primarily determined by the severity of the regurgitation, which is assessed by echocardiography. Mild regurgitation is often well-tolerated, and patients may remain asymptomatic for years. Moderate regurgitation can lead to gradual left ventricular enlargement and dysfunction over time.
Severe regurgitation, if left untreated, can lead to heart failure, arrhythmias, and sudden cardiac death.
Other factors that influence the prognosis of aortic regurgitation include:
- The underlying cause of the regurgitation: Rheumatic fever, infective endocarditis, and congenital heart defects are associated with a worse prognosis than degenerative aortic regurgitation.
- The patient’s age and overall health status: Older patients and those with other comorbidities have a higher risk of complications.
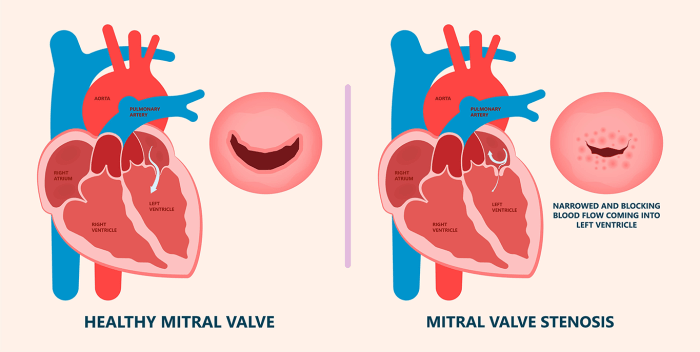
- The presence of associated valvular lesions: Patients with aortic regurgitation and concomitant mitral valve disease or aortic stenosis have a worse prognosis.
Long-Term Outcomes of Aortic Valve Surgery
Aortic valve surgery is the definitive treatment for aortic regurgitation. The long-term outcomes of surgery are generally good, with most patients experiencing significant improvement in symptoms and quality of life.
The 10-year survival rate after aortic valve surgery is approximately 80-90%. However, the risk of complications is higher in patients with severe regurgitation, those with other comorbidities, and those who undergo surgery at an older age.
The most common complications of aortic valve surgery include bleeding, infection, and arrhythmias. The risk of these complications can be reduced by careful patient selection, meticulous surgical technique, and appropriate postoperative care.
Case Study
A 65-year-old male with a history of hypertension and hyperlipidemia presents with a 6-month history of progressive dyspnea on exertion and palpitations.
On physical examination, he is afebrile, with a blood pressure of 150/90 mmHg, a pulse of 100 beats per minute and irregular, and a respiratory rate of 18 breaths per minute. Jugular venous distension is present, and there is a laterally displaced apical impulse.
Auscultation of the heart reveals a grade 3/6 holosystolic murmur at the left sternal border, radiating to the axilla. There is a diastolic murmur heard best at the third intercostal space along the left sternal border.
Diagnostic Workup
An electrocardiogram shows atrial fibrillation with a rapid ventricular response. A chest X-ray shows cardiomegaly and pulmonary vascular congestion. Echocardiography confirms severe aortic regurgitation with a regurgitant volume of 60 mL per beat. The left ventricle is dilated and hypertrophied, with an ejection fraction of 55%.
Treatment Plan
The patient is started on digoxin and furosemide to control his heart rate and volume overload. He is referred for surgical aortic valve replacement, which is performed successfully. The patient’s symptoms resolve postoperatively, and he is discharged home on a regimen of aspirin, warfarin, and lisinopril.
Outcomes
The patient has been followed up for 5 years since his surgery and has remained asymptomatic. His echocardiogram shows no evidence of aortic regurgitation, and his left ventricular function has remained normal.
Query Resolution
What are the key pathophysiological mechanisms leading to aortic regurgitation?
Aortic regurgitation can result from various mechanisms, including valvular abnormalities (e.g., bicuspid aortic valve, rheumatic heart disease), aortic root dilation (e.g., Marfan syndrome), and left ventricular dysfunction (e.g., ischemic heart disease).
How does aortic regurgitation affect cardiac hemodynamics?
Aortic regurgitation disrupts the normal flow of blood during diastole, leading to volume overload of the left ventricle. This can result in increased left ventricular end-diastolic pressure, decreased cardiac output, and compensatory mechanisms such as increased heart rate and stroke volume.
What are the common clinical manifestations of aortic regurgitation?
Patients with aortic regurgitation may present with a range of symptoms, including dyspnea, fatigue, palpitations, and chest pain. Physical examination findings may include a diastolic murmur, widened pulse pressure, and signs of heart failure.